Projects Experimental Virology

Principles of HCV assembly and entry and their role in virus persistence
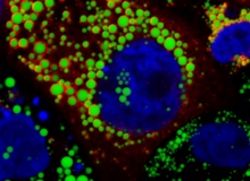
Fifty to 90% of HCV infections take a chronic course. The association of the virus with host-derived lipoproteins contributes to persistence via a direct influence on virus entry into liver cells and in addition through protection from antibodies. Lipoproteins consist of apoproteins like Apolipoprotein B or E (ApoB, ApoE) and lipids. They are synthesized in liver cells and secreted to transport lipids to different body cells and tissues. ApoE interacts with HCV particles and ApoE polymorphisms are associated with a different course of HCV infection. We analyze host factors and viral determinants that modulate viral association with lipoproteins in order to define their role for virus persistence. The interaction of HCV with lipoproteins is initiated during virus assembly which occurs at cellular lipid storage organelles, so called lipid droplets.
After virus release, circulating lipoproteins are incorporated into HCV particles (Bankwitz et al. J Hepatol 2017). This maturation facilitates virus attachment to liver cells and enhances antibody escape (Bankwitz et al. J Hepatol 2017). Funded by the CRC900 we explore cellular and viral proteins that mediate interaction of HCV with lipoproteins. Ultimately, the information how HCV uses lipoproteins to evade antibody responses should facilitate HCV vaccine development.
Publications

In a fraction of HCV patients, vigorous immune responses lead to control and elimination of the virus infection. Thus, some patients are able to mount protective immune responses against HCV. However, the precise features of protective immunity are not fully understood. Particularly the role of antibodies in protection from HCV is not clearly defined. Therefore, supported by the DZIF HCV-Vaccine project and the Helmholtz-Alberta Initiative of Infectious Disease Research (HAI-IDR), we explore the role of antibodies in protecting from HCV infection. Ultimately, we aim to translate this information into the development of an HCV vaccine candidate.
Publications

HCV has a narrow species tropism and naturally only infects humans. The determinants responsible for HCV´s species tropism are incompletely defined. Lack of immune competent small animal models is a major roadblock for HCV vaccine development, since a rigorous in vivo model for prioritization of vaccine candidates for costly clinical development is lacking. The inability of HCV to propagate in non-human cells may be due to lack or genetic incompatibility of essential viral replication co-factors and/or due to operation of antiviral restriction mechanisms effectively suppressing viral replication in non-human host cells. Taking this into account we employ both rationale as well as unbiased genetic screening systems to derive a comprehensive profile of all factors relevant to the species barrier for HCV infection of mouse cells. Ultimately, we will use this information to develop HCV in vivo models to facilitate vaccine development. This project was generously funded by an ERC starting grant (VIRAFRONT; 2012-2017) and it is now continued with funding from the Deutschen Zentrum für Infektionsforschung (DZIF)..
Publications
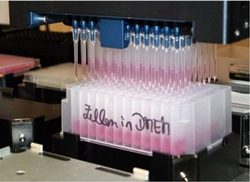
We develop and implement high throughput screening assays to identify molecules with antiviral activity against HCV and RSV. To this end we use luminescence or fluorescence-based reporter systems and compound libraries of the HZI, the MHH as well as external collaboration partners. These libraries comprise a large spectrum of chemical scaffolds including complex molecules from natural sources (bacterial secondary metabolites, plant-derived compounds) as well as licensed drugs. Using our expertise in basic virology we conduct mode of action studies and explore viral resistance mechanisms. Ultimately, these efforts are geared to contribute to the development for novel treatment options.
Publications
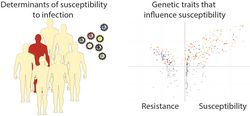
Some HCV patients naturally clear the infection, while the majority progress to chronicity. Moreover, the course of chronic infection is highly variable between patients. In RSV, most children have encountered a first infection within their first 18 months of life. A fraction of these children suffer from a severe course of infection. In both viral infections, the principles that govern disease susceptibility and severity are incompletely defined. This information, however, is important to provide optimal medical care and prophylaxis. Therefore, we team up with our clinical partners at the MHH, and explore principles of host susceptibility to these viral infections. These studies involve next generation sequencing technologies to monitor viral and host features and to determine the importance of host genetics in disease susceptibility. Through collaborations with physician scientists we have access to unique patient cohorts to investigate principles of virus pathogenesis in humans. This project is funded by the COALITION network and the iMed initiative. It is also part of the recently founded Centre for Individualized Infection Medicine (CIIM).
Publications
Principles of HCV assembly and entry and their role in virus persistence
Bankwitz D, Doepke M, Hueging K, Weller R, Bruening J, Behrendt P, Lee JY, Vondran FWR, Manns MP, Bartenschlager R, Pietschmann T (2017) Maturation of secreted HCV particles by incorporation of secreted ApoE protects from antibodies by enhancing infectivity. J Hepatol, pii: S0168-8278(17)30251-30259.
Vieyres G, Welsch K, Gerold G, Gentzsch J, Kahl S, Vondran FW, Kaderali L, Pietschmann T (2016) ABHD5/CGI-58, the Chanarin-Dorfman Syndrome Protein, Mobilises Lipid Stores for Hepatitis C Virus Production. PLoS Pathog 12(4): e1005568.
Gerold G, Meissner F, Bruening J, Welsch K, Perin PM, Baumert TF, Vondran FW, Kaderali L, Marcotrigiano J, Khan AG, Mann M, Rice CM, Pietschmann T (2015) Quantitative Proteomics Identifies Serum Response Factor Binding Protein 1 as a Host Factor for Hepatitis C Virus Entry. Cell Rep 12(5): 864-878.
Hueging K, Doepke M, Vieyres G, Bankwitz D, Frentzen A, Doerrbecker J, Gumz F, Haid S, Wolk B, Kaderali L, Pietschmann T (2014) Apolipoprotein E codetermines tissue tropism of hepatitis C virus and is crucial for viral cell-to-cell transmission by contributing to a postenvelopment step of assembly. J Virol 88(3): 1433-1446.
Gentzsch J, Brohm C, Steinmann E, Friesland M, Menzel N, Vieyres G, Perin PM, Frentzen A, Kaderali L, Pietschmann T (2013) hepatitis c Virus p7 is critical for capsid assembly and envelopment. PLoS Pathog 9(5): e1003355.
Determinants of protective immunity in HCV: A gold standard for vaccine development
Bartenschlager R, Baumert TF, Bukh J, Houghton M, Lemon SM, Lindenbach BD, Lohmann V, Moradpour D, Pietschmann T, Rice CM, Thimme R, Wakita T. Critical challenges and emerging opportunities in hepatitis C virus research in an era of potent antiviral therapy: Considerations for scientists and funding agencies. Virus Res. 2018 Mar 15;248:53-62.
Vasiliauskaite I, Owsianka A, England P, Khan AG, Cole S, Bankwitz D, Foung SKH, Pietschmann T, Marcotrigiano J, Rey FA, Patel AH, Krey T. Conformational Flexibility in the Immunoglobulin-Like Domain of the Hepatitis C Virus Glycoprotein E2. MBio. 2017 May 16;8(3).
Bankwitz D, Doepke M, Hueging K, Weller R, Bruening J, Behrendt P, Lee JY, Vondran FWR, Manns MP, Bartenschlager R, Pietschmann T (2017) Maturation of secreted HCV particles by incorporation of secreted ApoE protects from antibodies by enhancing infectivity. J Hepatol, pii: S0168-8278(17)30251-30259.
Bankwitz D, Pietschmann T (2016) Hepatitis C virus plays hide and seek with neutralizing antibodies. Hepatology 64(6): 1840-1842.
Bankwitz D, Vieyres G, Hueging K, Bitzegeio J, Doepke M, Chhatwal P, Haid S, Catanese MT, Zeisel MB, Nicosia A, Baumert TF, Kaderali L, Pietschmann T (2014) Role of hypervariable region 1 for the interplay of hepatitis C virus with entry factors and lipoproteins. J Virol 88(21): 12644-12655.
Doerrbecker J, Friesland M, Riebesehl N, Ginkel C, Behrendt P, Brown RJ, Ciesek S, Wedemeyer H, Sarrazin C, Kaderali L, Pietschmann T, Steinmann E (2014) Incorporation of primary patient-derived glycoproteins into authentic infectious hepatitis C virus particles. Hepatology 60(2): 508-520.
Bankwitz D, Steinmann E, Bitzegeio J, Ciesek S, Friesland M, Herrmann E, Zeisel MB, Baumert TF, Keck ZY, Foung SK, Pecheur EI, Pietschmann T (2010) Hepatitis C virus hypervariable region 1 modulates receptor interactions, conceals the CD81 binding site, and protects conserved neutralizing epitopes. J Virol 84(11): 5751-5763.
Mechanisms of HCV tissue and species tropism
Repressors of viral infection, WO2017/207725A1
von Schaewen M, Dorner M, Hueging K, Foquet L, Gerges S, Hrebikova G, Heller B, Bitzegeio J, Doerrbecker J, Horwitz JA, Gerold G, Suerbaum S, Rice CM, Meuleman P, Pietschmann T, Ploss A. Expanding the Host Range of Hepatitis C Virus through Viral Adaptation. MBio. 2016 Nov 8;7(6)
Anggakusuma, Brown RJ, Banda DH, Todt D, Vieyres G, Steinmann E, Pietschmann T (2016) Hepacivirus NS3/4A Proteases Interfere with MAVS Signaling in both Their Cognate Animal Hosts and Humans: Implications for Zoonotic Transmission. J Virol 90(23): 10670-10681.
Pfaender S, Grabski E, Detje CN, Riebesehl N, Lienenklaus S, Steinmann E, Kalinke U, Pietschmann T (2016) Hepatitis C Virus Stimulates Murine CD8alpha-Like Dendritic Cells to Produce Type I Interferon in a TRIF-Dependent Manner. PLoS Pathog 12(7): e1005736.
Anggakusuma, Frentzen A, Gurlevik E, Yuan Q, Steinmann E, Ott M, Staeheli P, Schmid-Burgk J, Schmidt T, Hornung V, Kuehnel F, Pietschmann T (2015) Control of hepatitis C virus replication in mouse liver-derived cells by MAVS-dependent production of type I and type III interferons. J Virol 89(7): 3833-3845.
Frentzen A, Anggakusuma, Gurlevik E, Hueging K, Knocke S, Ginkel C, Brown RJ, Heim M, Dill MT, Kroger A, Kalinke U, Kaderali L, Kuehnel F, Pietschmann T (2014) Cell entry, efficient RNA replication, and production of infectious hepatitis C virus progeny in mouse liver-derived cells. Hepatology 59(1): 78-88.
Frentzen A, Huging K, Bitzegeio J, Friesland M, Haid S, Gentzsch J, Hoffmann M, Lindemann D, Zimmer G, Zielecki F, Weber F, Steinmann E, Pietschmann T (2011) Completion of hepatitis C virus replication cycle in heterokaryons excludes dominant restrictions in human non-liver and mouse liver cell lines. PLoS Pathog 7(4): e1002029.
HCV and RSV antivirals
Labyrinthopeptins as anti-viral agents EPA16809653.5, pending
Diagnostics and therapy for human respiratory syncytial virus (hRSV) EP17195522.2, pending
Behrendt P, Perin P, Menzel N, Banda D, Pfaender S, Alves MP, Thiel V, Meuleman P, Colpitts CC, Schang LM, Vondran FWR, Anggakusuma, Manns MP, Steinmann E, Pietschmann T. Pentagalloylglucose, a highly bioavailable polyphenolic compound present in Cortex moutan, efficiently blocks hepatitis C virus entry. Antiviral Res. 2017 Nov;147:19-28.
Pietschmann T. Clinically Approved Ion Channel Inhibitors Close Gates for Hepatitis C Virus and Open Doors for Drug Repurposing in Infectious Viral Diseases. J Virol. 2017 Jan 3;91(2).
Perin PM, Haid S, Brown RJ, Doerrbecker J, Schulze K, Zeilinger C, von Schaewen M, Heller B, Vercauteren K, Luxenburger E, Baktash YM, Vondran FW, Speerstra S, Awadh A, Mukhtarov F, Schang LM, Kirschning A, Muller R, Guzman CA, Kaderali L, Randall G, Meuleman P, Ploss A, Pietschmann T (2016) Flunarizine prevents hepatitis C virus membrane fusion in a genotype-dependent manner by targeting the potential fusion peptide within E1. Hepatology 63(1): 49-62.
Haid S, Grethe C, Bankwitz D, Grunwald T, Pietschmann T (2015) Identification of a Human Respiratory Syncytial Virus Cell Entry Inhibitor by Using a Novel Lentiviral Pseudotype System. J Virol 90(6): 3065-3073.
Koutsoudakis G, Romero-Brey I, Berger C, Perez-Vilaro G, Monteiro Perin P, Vondran FW, Kalesse M, Harmrolfs K, Muller R, Martinez JP, Pietschmann T, Bartenschlager R, Bronstrup M, Meyerhans A, Diez J (2015) Soraphen A: A broad-spectrum antiviral natural product with potent anti-hepatitis C virus activity. J Hepatol 63(4): 813-821.
Anggakusuma, Colpitts CC, Schang LM, Rachmawati H, Frentzen A, Pfaender S, Behrendt P, Brown RJ, Bankwitz D, Steinmann J, Ott M, Meuleman P, Rice CM, Ploss A, Pietschmann T, Steinmann E (2014) Turmeric curcumin inhibits entry of all hepatitis C virus genotypes into human liver cells. Gut 63(7): 1137-1149.
Haid S, Novodomska A, Gentzsch J, Grethe C, Geuenich S, Bankwitz D, Chhatwal P, Jannack B, Hennebelle T, Bailleul F, Keppler OT, Poenisch M, Bartenschlager R, Hernandez C, Lemasson M, Rosenberg AR, Wong-Staal F, Davioud-Charvet E, Pietschmann T (2012) A plant-derived flavonoid inhibits entry of all HCV genotypes into human hepatocytes. Gastroenterology 143(1): 213-222 e215.
Host and viral factors that govern susceptibility to HCV and RSV
Diagnostics and therapy for human respiratory syncytial virus (hRSV) EP17195522.2, pending
Baier C, Haid S, Beilken A, Behnert A, Wetzke M, Brown RJP, Schmitt C, Ebadi E, Hansen G, Schulz TF, Pietschmann T, Bange FC. Molecular characteristics and successful management of a respiratory syncytial virus outbreak among pediatric patients with hemato-oncological disease. Antimicrob Resist Infect Control. 2018 Feb 13;7:21.
Weller R, Hueging K, Brown RJP, Todt D, Joecks S, Vondran FWR, Pietschmann T (2017) Hepatitis C virus strain-dependent usage of apolipoprotein E modulates assembly efficiency and specific infectivity of secreted virions. J Virol. pii: JVI.00422-17.
Vieyres G, Welsch K, Gerold G, Gentzsch J, Kahl S, Vondran FW, Kaderali L, Pietschmann T (2016) ABHD5/CGI-58, the Chanarin-Dorfman Syndrome Protein, Mobilises Lipid Stores for Hepatitis C Virus Production. PLoS Pathog 12(4): e1005568.
Hedenstierna M, Weiland O, Brass A, Bankwitz D, Behrendt P, Uhnoo I, Aleman S, Cardell K, Fryden A, Norkrans G, Eilard A, Glaumann H, Pietschmann T, Sallberg M, Brenndorfer ED (2015) Long-term follow-up of successful hepatitis C virus therapy: waning immune responses and disappearance of liver disease are consistent with cure. Aliment Pharmacol Ther 41(6): 532-543.
Doerrbecker J, Friesland M, Riebesehl N, Ginkel C, Behrendt P, Brown RJ, Ciesek S, Wedemeyer H, Sarrazin C, Kaderali L, Pietschmann T, Steinmann E (2014) Incorporation of primary patient-derived glycoproteins into authentic infectious hepatitis C virus particles. Hepatology 60(2): 508-520.
Haid S, Grethe C, Dill MT, Heim M, Kaderali L, Pietschmann T (2014) Isolate-dependent use of claudins for cell entry by hepatitis C virus. Hepatology 59(1): 24-34.